Irenea, neurological rehabilitation institute
The Neurological Rehabilitation Institute Irenea is a highly specialised centre in rehabilitation of people with acquired brain injury or other neurological disabilities.
We provide expert, personalised attention with the highest human, scientific and technical level, to achieve the greatest autonomy and independence possible of the patient
With a person-oriented philosophy and a cross-disciplinary treatment model, we have developed intensive treatment programmes to meet the needs of each patient depending on his or her specific problem or disorder.
These programmes are periodically assessed to determine the patient’s progress in the rehabilitation and to modify the programme’s objectives.
Why rehabilitate in irenea?
We have multidisciplinary team of professionals high specialized in the field of neurorehabilitation:
- Neurologist
- Rehabilitation doctor
- Neuropsychologist
- Speech therapists
- Occupational therapists
- Physiotherapists
- etc.
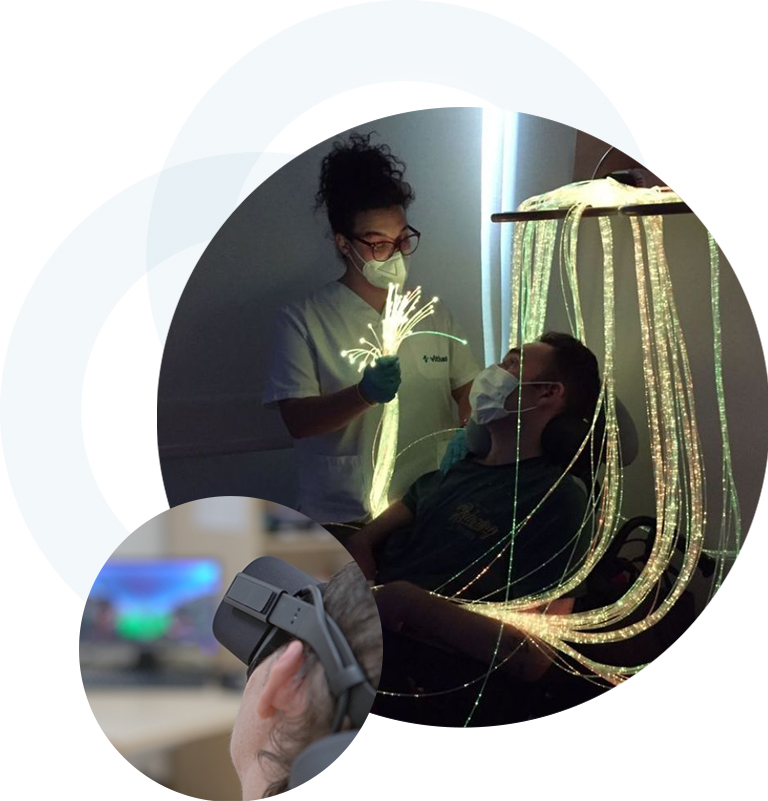
We carries out intense scientific and researchin the field of neurorehabilitation and technologies applied to personal autonomy in particular.
We provide the latest and most news technological, robotic and clinical solutions to our patients, most of them developed by our researcher.
We achieved an average of 95% of the objectives set by the rehabilitation team on admission.
Neurorehabilitation
Our treatment of patients with acquired brain injury (ABI) and other neurological injuries should is early, individualized, intensive, and cross-disciplinary
Among the most frequent pathologies that we attend are:
- Acquired Brain Damage
- Cranioencephalic Trauma (traffic accidents, work accidents, sports accidents, falls, etc.)
- Cerebrovascular accidents (ischemic strokes, hemorrhagic strokes, thrombosis, embolism …)
- Cerebral anoxic-ischemic pathology (cerebral anoxia due to cardiorespiratory arrest)
- Infectious brain pathology (meningitis, encephalitis, etc.)
- Brain Tumors
- Degenerative diseases (Parkinson’s, Multiple Sclerosis, etc.)
- Cerebral palsy
- Neurodevelopmental disorder
Pediatric neurorehabilitation
Our pediatric neurological unit is aimed at the child and youth population with or at risk of suffering complications in their development.
Irenea’s aim is to get a head start in the race to recover a pace of development that allows these children to lead well-rounded personal, family, and social lives.
We achieve the highest degree of autonomy for the child and enhance the development of his or her skills.

Disorders of consciousness unit
Irenea Vithas has the Unit of Altered States of Consciousness, unique in Spain, where the patient will always have a customized plan based on their status and their needs.
This Unit of Coma, Non-Responsive Vigil Syndrome / Vegetative State, State of Minimum Consciousness, Locked in / Captivity Syndrome, it makes an accurate diagnosis, an evolutionary prognosis and a specialized treatment with the use of the latest techniques and new experimental drugs.
With a professional team dedicated exclusively to comprehensive rehabilitation of people with severe neurological pathologies
Forms of treatment
We provide an intensive, specialized and individualized treatment to adapt to the specific needs of each patient, whether adult or child, both on an outpatient basis and on an admission basis.
In Irenea Vithas, to meet the needs of the patient and his or her family, the Neurological Rehabilitation Institute offers two forms of treatment.
Residential unit
The patient remains in the hospital in an individual personalized room and receives morning and afternoon rehabilitation sessions
Outpatients unit
Patients are cared for as outpatients during the morning or the afternoon from Monday to Friday.

International department
Irenea offers a wide range of medical services, providing patients with comprehensive care always taking into consideration their individual needs.
We know how important the support during treatment is, especially when one is outside his or her home country.
If you want to contact Vithas Hospitals in order to schedule a visit to the doctor, diagnosis, treatment or for any other inquiries, please contact us through on-line contact form.
Upon your request, the staff of the International Department will contact you for the details of your medical history, diagnosis and previous treatments.
Possibly, we will ask you to send us by email images of diagnostic tests, discharge reports, results of clinical analysis and other supplementary material, which will be used by our experts to evaluate you clinical case.
After you case has been evaluated, we will send you a budget for diagnosis and treatment accompanied by a detailed explanation.
Our services
Translation, interpretation and guidance
Treatment planning according to diagnosis
Medicalized aircraft
Provide estimates of the cost of medical services
Visa arrangements
Accommodation arrangement
Translation of the discharge report, results of tests and examinations, as well as additional documents required
* The International Department coordinators select a specialist individually depending on each case, prepare and organize the medical program provide estimates of the costs of treatment, issues an invitation for visa formalities and provide their customers with all necessary support before, during and after their stay in the hospital.
** During hospitalization or visit to a doctor, the patient will have an individually selected professional translator. Upon patient’s request, the International Department will organize a shuttle or ambulance in cases that require reanimation. If the patient comes for treatment in severe health conditions, our staff will organize an emergency ambulance service from airport to the hospital. At the airport the patient will be attended by a team of doctors ready to apply resuscitation protocols at any time when needed

